early clamping of the umbilical cord -- done with the aim of transferring the
infant to a specialist and maintaining a sterile field for prompt suturing of
incisions made for episiotomy or Caesarean delivery. Meanwhile, advocates
of what Apgar referred to as "slow birth" continued a long tradition of
measuring the amount of placental blood an infant got if the cord was left
unclamped until pulsations in it ceased.
the placenta through the umbilical arteries, and cease when pulmonary
respiration is fully established with closure of the foramen ovale and ductus
arteriosus in the heart (Dawes et al. 1953).
newborn lambs. These experiments did involve "tying the cord," which might
explain the finding of a pattern of "neonatal circulation" intermediate between
that of the fetus and that of the adult. Born et al. (1954) found the ductus
arteriosus begins to close within 5 to 15 minutes of pulmonary ventilation with
continuing constriction for several minutes, but remained partially patent for
12 hours or more. The foramen ovale, on the other hand, closes within a
minute following birth, forcing circulation to the lungs.
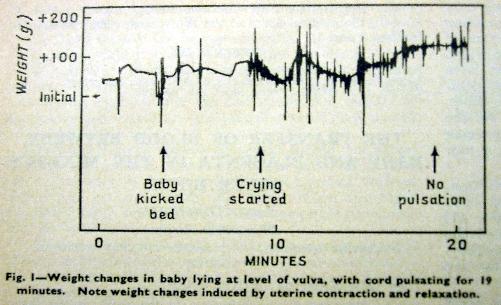
umbilical cord intact allowing ongoing placental circulation. Fluctuations in
weight occurred in response to uterine contractions, elevation of the baby
above or below the mother's uterus, and pulsations of the cord.
gain/loss tracings. In figure 1 (below) postnatal activity and weight profile are
shown for a baby who started crying only 9 minutes after birth, and with
pulsations of the cord continuing for 19 minutes after birth.
been cut within the first minute after birth?
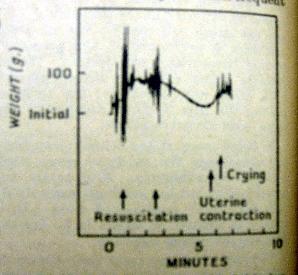
resuscitation was started
within one minute on an infant
described as "slow to cry."
Crying began more than 6
minutes after birth following a
uterine contraction and
additional weight gain from
placental blood. Pulsations
of the cord continued
throughout the 10 minute
interval shown in the graph.
This would surely have been
another infant described as
severely depressed by
Apgar, and with an ominous
outcome.
left untied, a baby will usually increase his blood volume by a significant
amount." She compared her findings to those of Haselhorst (1929) and
Allmeling (1930), noting that placental transfusion increased a newborn's
weight by by 0.8 to 4.7 percent, which (assuming blood volume is about 10
percent of an infant's weight) amounts to as much or more than 40 percent of
the baby's blood volume.
membrane syndrome, was a major concern, and quite widely attributed to the
new vogue of early umbilical cord clamping. Gunther commented that even
while pulsations of the cord continued, cessation of placental transfusion was
often apparent, "as if a main reservoir had been filled," and she cited the
research of Jaykka (1957) who determined that inflation of the lungs occurred
with increasing blood flow into the alveolar capillaries - the shift of blood
volume from the placenta to the lungs.
blood could cause severe jaundice. She noted, however that only one of the
50 babies in her study developed jaundice - and it should be noted that
bilirubin levels are normally high in newborn infants. Several investigators of
erythroblastosis fetalis had already for many years observed that bilirubin only
gets into the brain if the blood-brain barrier is compromised by anoxia or
sepsis (Orth 1875, Schmorl 1904, Zimmerman and Yannet 1933). Lucey et al.
(1964) would later demonstrate that bilirubin stains only the subcortical nuclei
susceptible to damage in monkeys subjected to experimental asphyxiation at
birth.